Here are some illustrations of the work we have done.
Together they demonstrate the benefits of using our unique Personal Injury Formulation and Intervention Model (PIFIM). More on this model in due course.
1. A treating psychology adult client
She has a complicated family background growing up in China where her family largely still were. M’s family would request financial support which she was not happy about, yet she was fearful of being perceived as selfish. Meeting her family’s needs was an important value to her. She struggled to maintain relationships – personal and professional – and feared being lonely should her family disown her; her insight resulted in bouts of low mood and anger. The professional teams felt stuck and concerned about her emotional wellbeing and risk.
Using our unique formulation and intervention model – PIFIM – the PsychWorks Associate treating psychologist supported M to develop her insight about herself and her life experiences. This insight then allowed the team to develop goals, unpick risks, and support her with accessing input from her social and professional networks. Training for the care and therapy teams was also provided to understand how relationships could be perceived and how to offer support to M which increased her sense of belonging. Culture-sensitive, formulation-led team meetings resulted in greater understanding of M’s past and injury-related traumas. This formulation allow the team to monitor her financial risk in a way that felt safe to M. M’s case settled with her living a life less fearful of family pressure with a range of personal and carer relationships she was able to sustain with positive goal outcomes.
2. A treating psychology paediatric client
Client J is a 15 year old male with his mother and adult sister. J has high-average intelligence, but is not interested in academic achievement nor wanting to exert or apply himself too hard. He loves computer games, fast cars and animals. Neither he, nor his family enjoy exercise.
Five years ago, J was injured in a road traffic collision when he was 10. His motor cortex was affected making it difficult for him to physically mobilise independently so he used a wheelchair when walking became too hard. He also had some symptoms of dysexeutive syndrome (impulsivity, difficulty planning, organising and regulating emotions) but these were mild. He appeared to have retained most of his intellectual ability and passed his 11+ with flying colours. However, he was uninterested in academic achievements or exerting himself too hard physically or emotionally. Like his family, he enjoyed playing computer games. He was using his wheelchair more and more.
J was referred to PsychWorks Associates treating psychology team because he was refusing to engage in any rehabilitation activities at the gym and at school, and his family were unable to set appropriate boundaries to motivate him and the support workers were unclear about how to support him. His physiotherapist feared he could lose the ability to walk.
Using the models around grief, J was understood in his journey post-injury. He revealed that he felt his team did not care about how he felt and thought their targets were unrealistic. Our Psychology Associate helped him identify what would be a more realistic goal and set up joint meetings with his MDT to hear his opinion. Thinking about family culture with the professional team and improving outcomes, the goals and how they were offered were adapted to be more motivating, such as to purchase sweets or computer games from the shop rather than go to the gym or walk around school. Both he and his team were able to minimise input by producing an interdisciplinary approach that covered a range of physiotherapy, personal trainer and OT goals which were implemented by the well-trained care team in single visits out several times a week. J reported finding the level of functional rehabilitation much more meaningful and less threatening than some of the gym- and home-based tasks he was asked to complete.
J is a 15 year old male with his mother and adult sister. J has high-average intelligence, but is not interested in academic achievement nor wanting to exert or apply himself too hard. He loves computer games, fast cars and animals.
Neither he, nor his family enjoy exercise.
Five years ago, J was injured in a road traffic collision when he was 10. His motor cortex was affected making it difficult for him to physically mobilise independently so he used a wheelchair when walking became too hard. He also had some symptoms of dysexeutive syndrome (impulsivity, difficulty planning, organising and regulating emotions) but these were mild. He appeared to have retained most of his intellectual ability and passed his 11+ with flying colours. However, he was uninterested in academic achievements or exerting himself too hard physically or emotionally. Like his family, he enjoyed playing computer games. He was using his wheelchair more and more.
J was referred to PsychWorks Associates treating psychology team because he was refusing to engage in any rehabilitation activities at the gym and at school, and his family were unable to set appropriate boundaries to motivate him and the support workers were unclear about how to support him. His physiotherapist feared he could lose the ability to walk.
Using the models around grief, J was understood in his journey post-injury. He revealed that he felt his team did not care about how he felt and thought their targets were unrealistic. Our Psychology Associate helped him identify what would be a more realistic goal and set up joint meetings with his MDT to hear his opinion. Thinking about family culture with the professional team and improving outcomes, the goals and how they were offered were adapted to be more motivating, such as to purchase sweets or computer games from the shop rather than go to the gym or walk around school. Both he and his team were able to minimise input by producing an interdisciplinary approach that covered a range of physiotherapy, personal trainer and OT goals which were implemented by the well-trained care team in single visits out several times a week. J reported finding the level of functional rehabilitation much more meaningful and less threatening than some of the gym- and home-based tasks he was asked to complete.
3. A case management paediatric client
The impact of 9-year-old Sudanese Client O’s near total hypoxic ischaemic brain injury at birth meant that school was poorly attended due to anxiety. The case manager used our PsychWorks Associates’ PIFIM model as part of an immediate needs assessment to understand that his anxieties were related to falling due to his hearing loss and hemiplegia. These were heightened by a series of health appointments related to planned surgery in a few months’ time which his whole family were preoccupied by. It was also challenging for his parents to contain the pressures of their son’s rehabilitation goals when the litigation timetable was busy.
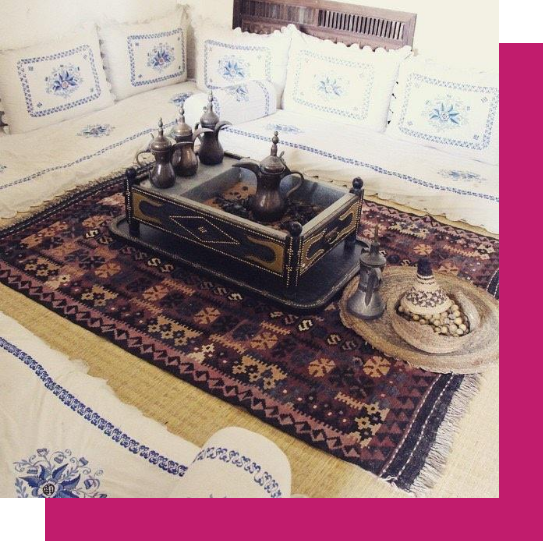
Additionally, his mother, his main caregiver, experienced a complicated labour which she described as traumatic because the non-Sudanese midwife seemed to ignore her distressed cries for help despite tending to other women. This made it harder for her to trust professionals which manifested as tearfulness and anger at times. The parents stated a preference for a care team that could represent their Sudanese cuisines and language. This was key as their son liked Sudanese foods and preferred to speak Arabic, therefore, members of the family’s community were formally made carers.
With PIFIM, the case management team was able to understand the client’s distress in terms of an overwhelmed family system that needed support in order to minimise the anxiety exhibited by O. Key recommendations for the whole team driven by PIFIM’s mediating factors included a) offering trauma and culture training amplifying the family’s needs while also meeting the necessary care standards, b) holding supervision and team meetings to support appropriate boundary setting between the mother and carers to ensure safe working, c) communicating to the team around the client’s the legal timetable so input could be adjusted accordingly, and, d) basing all formal meetings on PIFIM to document improvement and share changes, e) providing psychological support to help parents respond helpfully to their son should be available, f) encouraging joined-up discussions and work across the clinicians which was reflected in clinicians’ update reports.