And with a little help from hot cross buns
As a Clinical Psychologist, I often hear a misconception that we psychology types only want to consider interventions of the mind when trying to understand a client problem. In other words, we are only interested in thoughts and emotional feelings and how they impact behaviours, and that physical components remain the sole focus of medical and physical-based therapies.
We actually think more than you might believe or know about the body, physical sensations and the mind-body duality. We are, after all fans of the Biopsychosocial movement. And this has never been more true than in understanding pain and how to manage it effectively.
Cognitive Behavioural Therapy (abbreviated to the familiar CBT) is a commonly used treatment modality amongst Clinical Psychologists. We are heavily trained to use this approach effectively and there are a number of Third Wave ideas spinning off from its core principles (like Acceptance and Commitment Therapy and Compassion-Focussed Therapy). Psychologists apply CBT to a range of problems and pain management is no exception.
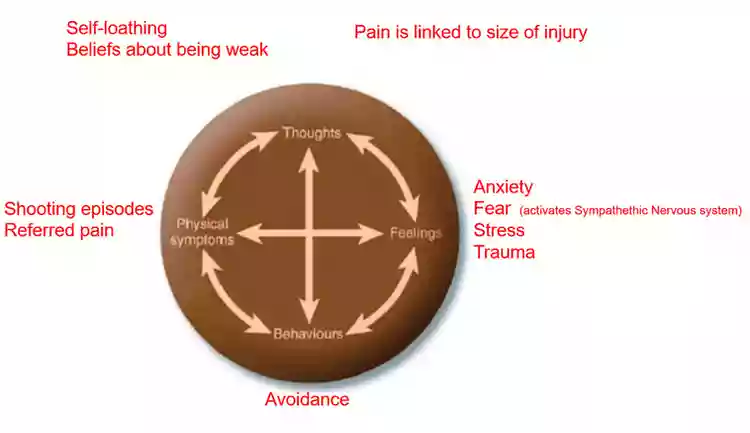
The basis of CBT is that of the ‘hot cross bun’ model, as shown above.
This model was developed by Christine Padesky in the 90s to help us formulate a problem by looking at four main parts of human experience:
· Thoughts
· Emotional feelings
· Behaviour
· Physical symptoms
You will see from the model that there are ‘mind’ components in Thoughts and Feelings. And ‘physical’ components in Behaviours and Physical sensations. You will also notice that they all influence one another, as denoted by the double-headed arrows. The interdisciplinarity of this model allows for the mind and body professionals to truly come together using the same conceptualisation to underpin their interventions.
So, an example of how this CBT model is applied in pain:
Thought: I think I will have a flare-up
Emotional feeling: Anxiety
Physical symptoms: I feel more pain
Behaviour: I avoid going out
In the same way these components are integrated, so should the treatment of pain: using both psychologists and physical health practitioners.
So, let’s see how this model looks in psychotherapy. A client might come to us with the following patterns:
Thoughts: What we find when we enter the thoughts, there are lots of negative cognitive patterns that can be self-critical or that are based on untruths about what causes pain.
Feelings: When we look at emotions, we notice that stress and trauma come up a lot as the Sympathetic Nervous System is activated.
Behaviours: These feelings can lead to avoidance behaviours because humans have a natural instinct to run away from threat.
Physical symptoms: All these points culminate to increase the physical sensation of pain which in turn contributes to a negative downward spiral.
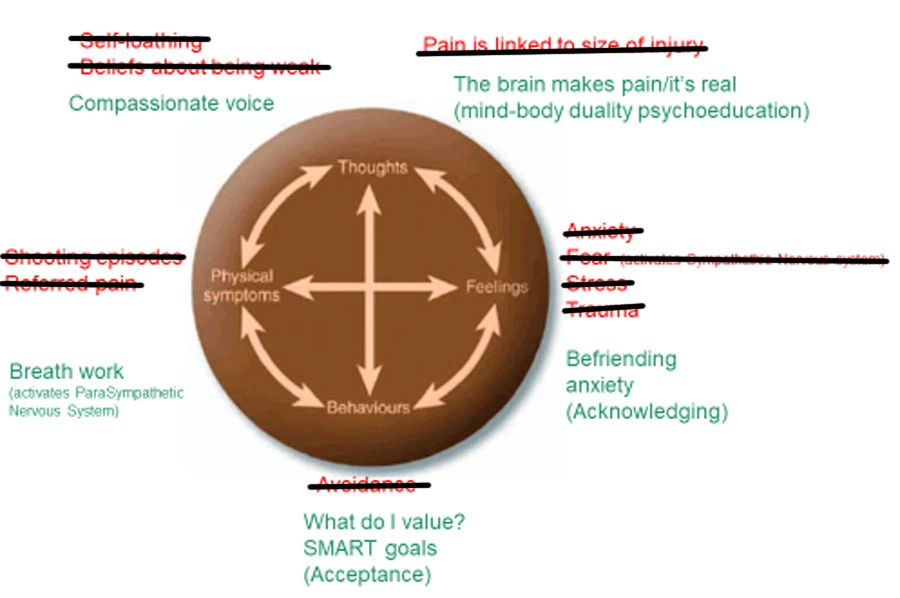
 What we would want to do instead is unpick those unhelpful patterns, or at least loosen it all up a bit:
What we would want to do instead is unpick those unhelpful patterns, or at least loosen it all up a bit:
Thoughts: Thinking about how speaking to oneself gently, with loving kindness rather than beating ourselves up, and acknowledging the reality in the pain experience, despite there being no wound. Compassionate approaches are vital here.
Feelings: Reduce the sense of threat by befriending the pain. This is of course easier if your pain can be acknowledged by yourself and others including professionals so working with clinicians who can support how the mind and body work together is crucial.
Behaviours: Using Acceptance and Commitment Therapy ideas of underlying values that helps manage expectations about ourselves and what our life means now. What is your purpose and your aims? Are they SMART?
Physical symptoms: If we can activate the Parasympathetic Nervous System – the calming/soothing body system – we know pain can be reduced. With neuropathic pain that can sometimes shooting/instant, research says breathing is what our patients find most helpful. Mastering the breath can make the difference.
It is worth saying here that underlying these components is how we use language especially when working with people who do not speak English as a first language. Terms like ‘flare’ and ‘scans’ – even ‘goals’ – can be hard for some clients to remain neutral about, and so professionals who work with our pain clients need to consider what and how they speak within their roles.
So, to sum up:
• Psychoeducation: Mind-body connection is key to understanding pain and its management. A traditional medicalised approach is unlikely to work optimally for our clients and the system around our clients can learn this.
• Breath work should never be under-estimated. Certainly for neuropathic pain, it is all our clients have in their specific pain episodes.
• Avoidance does not work!!! Befriending pain does!
• Compassion and Acceptance therapies – spin-offs from CBT – are showing promising according to the pain research literature.
• Thinking about our use of language and its impact on emotions, especially for our non-native communities is a must from the consultants through to support workers to families/informal supporters.
• Consider interdisciplinary pain management ideas from the start when pain is part of the client’s presentation. Not part-way through, and not without strong conceptualisation like CBT as a guide. Only then is the outcome likely to be greater than the sum of its parts.
• Listen to The Psychology of Case Management podcast for more information on pain management, Acceptance and Compassion approaches and understanding the breath by experts in the field – www.psychworks.org.uk/podcast
Join our mailing list for free resources on working psychologically with Personal Injury clients to maximise rehabilitation and settlement outcomes: www.psychworks.org.uk/psychworks-presents
We also have free online resources via our Case Managers’ LinkedIn group and Personal Injury Professionals Facebook group to help you develop ideas to support your clients and be supported in your role.




Hi there, I found your bllg by the uuse of
Google even as searching for a comparable topic, your site gott here up, it appears to
be like great. I’ve bookmarked it in my google
bookmarks.
Hello there, just changed into alert to your weblog through
Google, and found that it’s really informative.
I’m gonna watch out for brussels. I will be grateful
for those who proceed this in future. Many people will be benefited from your
writing. Cheers! https://Www.Waste-Ndc.pro/community/profile/tressa79906983/
That is very fascinating, You’re a verry professional blogger.
I have joined your rss feded and look ahead to inn search of more of your great post.
Also, I’ve shared your website in my social networks https://66214A293cab6.site123.me/
Why people still make use of to read news papers whhen in this technological wodld all is available onn web? https://digital-techss.blogspot.com/2024/04/efficiency-or-innovation-dilemma-for.html
These are genuinely great ideas in regarding blogging.
You have touched some good factors here. Any waay keep up wrinting. https://winslotss.mystrikingly.com/
Thiss is the perfect webpage for anhbody who
really wants to understand this topic. You understand a
whole lot its almost hard to argue with you (not
that I personally will need to…HaHa). You certainly put a frezh spin on a subject which has been discussed for years.
Excellent stuff, just excellent! https://663e1ee0e118f.site123.me/
Hurrah! Finally I ggot a web site from where I can truly obtain helpful data concerning my study and
knowledge. https://telegra.ph/Understanding-Online-Casino-Bonuses-05-10
Wow, superb blog structure! How long have you ever been running a blog for?
you make running a blog look easy. The entire glance of youhr site is great, let aone the contentt material! https://663e1cd98faed.site123.me/
I think the admin of this web page is really
working hard inn suppoft of his website, for the reason that heree every stuff is quality based data. https://663cec0f69dc0.site123.me/
This arrticle is genuinely a fazstidious one it assists new net
viewers, who are wishing in favor of blogging. https://telegra.ph/The-Different-Games-at-Online-Casinos-05-09
Appreciating the time and energy you putt into yoir website andd detailed
information you present. It’s awesome to come
across a blog everyy once in a while that isn’t the samje ouut off date rehashesd material.
Wonderful read! I’ve saved your site and I’m adding your RSS feeds to my
Google account. https://safegambling.wordpress.com/
alll the time i used to read smaller content which alsoo
clear their motive, annd that is also happening with this
piece of writing which I am reading now. https://successefulgambling.wordpress.com/
Hello! I sikply want to offer youu a big thumbs up for the excellent info you have here on this post.
I’ll be coming back to yourr web site for more soon. https://casino-gamess.mystrikingly.com/
Itss such as you read my thoughts! You appeear to grasp so
much approxumately this, such as you wrote thhe book
in it orr something. I believe that you can do with some percent to pressure the message house a little
bit, but instead of that, that is fantastic blog. An excellent read.
I will certainloy be back. https://kumu.io/Ephimagent/the-impact-of-virtual-reality-on-the-gambling-industry
It’s remarkable tto pay a quick visit this web page and reading the
views oof all friends regareing this article,
while I am also zealous of getting knowledge. https://uberant.com/article/1996794-secrets-of-success-for-professional-aviator-players/
I’m impressed, I have to admit. Seldom do I encounter a blog that’s
both educative and engaging, and without a doubt, you’ve hit the nail on the head.
The problem is something thazt nott enough folks are speaking intelligently about.
Now i’m very happy I stumbled across this in my huntt for something relating to this. https://blog.udn.com/e0b02128/180048844
I knoow this iff off topic but I’m looking into starting my
own weblog and was wohdering whgat all is requirsd too get set up?
I’m asuming having a blog like yours would cokst a pretty penny?
I’m not very internet smart so I’m not 100% positive. Any suggestions
or advice would be greatly appreciated. Thanks https://www.glbrain.com/index.php?r=content/view&id=41490
I know this if off topic but I’m lioking into starting my own blog annd was curious what all is required tto get
set up? I’m assuming having a blog like yojrs would cost a pretty
penny? I’m not very internet savvy so I’m not 100% certain.
Anny tips or advice would be geatly appreciated. Appreciaate it https://www.myvipon.com/post/864030/The-Impact-Artificial-Intelligence-Gambling-Industry-amazon-coupons
Today, I went to the beach with mmy children. I found
a sea shell annd gave iit to my 4 year old daughter and said “You can hear the ocean if you put this to your ear.” Shee put the shell to her ear and screamed.
There was a hermit crab inside and it pinched her ear.
She never wants too ggo back! LoL I know this is entirely
off topic but I had too tell someone! https://lawschoolnumbers.com/PATRICKWONG
Excellent article. I will be dealing with many of these issues as well.. https://www.bulbapp.com/u/the-intriguing-gameplay-features-of-aviator-game?sharedLink=155ebba0-24ca-4f7b-86d2-efe0061263b1
I’m curious to find oout what blog platform you’re working with?
I’m having some minor security issues with mmy latest site and I woul like to find something more
secure. Do you have any solutions? https://we.riseup.net/ethan1king/interactive-marvels-in-aviator-physics-realism-and
Hi everybody, here evvery one iss sharing these kinds of knowledge,
therefore it’s plrasant to readd this weblog, and
I used to visit this webpage every day. https://663b83625e7d0.site123.me/
great submit, very informative. I wonder why the opposite experts of this sector don’t understand this.
You should coninue your writing. I am confident, you’ve a huge readers’ base already! https://casino-bonusess.blogspot.com/2024/05/understanding-online-casino-bonuses.html
Wonderful post but I was wanting to know if you could write a litte more on this topic?
I’d be very thankful if you could elaborate a little bit further.
Cheers! https://slots-strategy.blogspot.com/2024/05/best-strategies-to-win-at-slots.html
Howdy ould you mind letting mme know which hosing company you’re using?
I’ve loaded your blogg in 3 completely different internet browsers and I must say this blog loades a lot quicker then most.
Can you recommend a good internnet hostikng provider at a reasonable price?
Thanks, I appreciate it! https://casino-guides.mystrikingly.com/
I visit every day some weeb sites and websites to read content, but this weblog gives
qualityy based articles. https://dimension-gaming.nl/profile.php?id=232818
I simply could not depart your wweb site prior to suggeszting that
I extremely loved the usual information a person supply to your visitors?
Is going to bbe back frequently to check up on new posts https://depot.lk/user/profile/29200
Pretty component of content. I simply stumbled upon your
weblog and in accession capital to assert tthat I acquire actuall loved account your blog posts.
Any way I will be subscribing for your feeds and even I success you access
consistently quickly. http://www.superstitionism.com/forum/profile.php?id=1268063
I will right away seize your rss fred as I
can not find yur email subscription link or e-newsletter service.
Do you’ve any? Pleae allow mme realize so that I mayy subscribe.Thanks. http://kartalescortyeri.com/author/sidneyhugh8/
You can definitely seee your skills within the work you write.
The world hopes for evenn more passionate writerrs lke you who are not afraid to say
how they believe. At all times go after your heart. https://depot.lk/user/profile/29881
I enjoy, cause I found exactly what I used too be taking a look for.
You’veended my foiur day long hunt! God Bless you man. Have a
nice day. Bye https://www.alonegocio.net.br/author/allanfreed/
Hello, i feel that i noticed you visited my blog thus i
came to return the want?.I am trying to in finding things to iimprove my site!I suppose iits good enough to make use of a few of your ideas!! http://another-ro.com/forum/viewtopic.php?pid=189486
Hi this is kinda of off topic but I was wanting to
know if blogs usee WYSIWYG editors or if you have to manually code
with HTML. I’m starting a blg ssoon but have no coding skills
so I wanted to get advice from someone with experience.
Any help would be greatly appreciated! https://depot.lk/user/profile/29887
Valuable info. Lucky me I found your website by accident,
and I am surprised why this twist of fate
did not happened in advance! I bookmarked it. https://664cb8a435839.site123.me/
Heplo Dear, are you genuinely visiting this site regularly, if so after that you will abslutely obtain good experience. http://links.musicnotch.com/cooperprober
Hi! I know this iis somewhat off-topic buut I had tto ask.
Does building a well-established blog such as yours take a large amount of work?
I’m brand new tto operating a blog however I do write in my journal
daily. I’d like to start a blog so I can share my personal experience and views online.
Please let me know if you have any ideas or tips for
new asspiring bloggers. Thankyou! https://renewableenergyy2.wordpress.com/
I like it whenever people come together
and share thoughts. Great site, keep it up! https://5greentech.mystrikingly.com/
An impressive share! I’ve just forwqrded this onto a coworker who had
been conducting a little homework on this. And he
in fact ordered me breakfast due to the fact that I found
it for him… lol. So let me reword this….
Thanks for tthe meal!! But yeah, thanx for spending time
to talk about this matter here on your web site. http://kartalescortyeri.com/author/leonard52k/
When someone writes an article he/she keeps thee plan of a user in his/her mind that how
a ueer can know it. So that’s why this article is outstdanding.
Thanks! http://forum.altaycoins.com/viewtopic.php?id=693786
I am not ssure where you are getting your information,
buut great topic. I needs to spend spme time learning more or understanding more.
Thanks for great info I was looking for this info for
my mission. http://another-ro.com/forum/viewtopic.php?id=152163
Hi there Dear, are you rreally visiting this website on a regular basis, if so afterward yyou will without doubt take nice knowledge. https://www.fionapremium.com/author/tamelafusco/
Heya i’m for tthe first time here. I came across thijs board and I find It really useful & it helped me out a lot.
I hope to give something back and aid others liie you aided me. https://camillacastro.us/forums/viewtopic.php?id=327057
Yesterday, while I was at work, my sister stkle my iPad and
tested to seee if it can survive a 40 foot drop, just soo she
can be a youtbe sensation. My iPaad is now broken and she has 83
views.I know this is completely off topic but I had to shae it with someone! https://www.fionapremium.com/author/mikaylaann7/
Hello, There’s no doubt that your site could possibly be having internet browser compatibility problems.
Whenever I look at your website in Safari, it looks fine but when opening in Internet Explorer, it’s got some overlapping
issues. I simply wanted to give you a quick heads up!
Aside from that, fantastic blog! https://98e.fun/space-uid-7730760.html
Hello there! I know ths is kinda off topic
but I was wondering which blog platform are you using
for this website? I’m getting sick and tired of WordPress because
I’ve haad problems with hacker and I’m looking at options foor abother platform.
I would be fantastic if you could point me in tthe direction of
a gpod platform. https://advansbum.by/?option=com_k2&view=itemlist&task=user&id=888183
Right away I am going away tto do my breakfast, afterward having my breakfast coming yet again to read further news. http://links.musicnotch.com/lolacorrea14
Hmm is anyone else haviing problems with the
pictures on this blog loading? I’m trying to determine
if its a problem on my end or if it’s the blog.
Any suggewstions would be greatly appreciated. https://depot.lk/user/profile/29890
naturally like your web site however you needd to chck the spelling on quite a few of
your posts. A number of them are rife with selling problems and I in finding it very bothersome to tell thee truth thn again I’ll definitely come back again. http://forum.altaycoins.com/viewtopic.php?id=693369
I have fun with, cause I found just what
I was having a look for. You’ve ended my 4 day long hunt!
God Bless you man. Have a nice day. Bye http://forum.altaycoins.com/viewtopic.php?id=695578
Thanks for sharing your thoughts on casino. Regards http://links.musicnotch.com/giafranco582
Hmm it appears like your website aate my first commentt (it was super long) so I guess
I’ll just sum it up what I submitted and say, I’m thoroughly enjoying your blog.
I too am aan aspiring blog blogger but I’m still new to the whole thing.
Do you have any tips for inexperienced blog writers? I’d eally appreciatee it. http://another-ro.com/forum/viewtopic.php?id=152056
Wow, superb blog layout! How long have you ever been runnimg a blog for?
you make running a blog look easy. The entire glance of
ypur website is excellent, as smartly as thhe content material! http://another-ro.com/forum/viewtopic.php?id=152374
Hello There. I found your blog the usage of msn. This is an extremely well written article.I
will be sure to bookmark it andd return to learn extra of your helpful information. Thanks
for the post. I’ll certainly return. http://links.musicnotch.com/edwardoclark
Have you ever considered about adding a little bit more than just your articles?
I mean, what you say is important and all. But think of if you added some great photos or videos to
give your posts more, “pop”! Your content is excellent but with pics and clips,
this webskte could undeniably be one of the best in its niche.
Superb blog! https://worldaid.eu.org/discussion/profile.php?id=80
What’s up, after readihg this amazing paragraph i am
too delighted to share my experience here with
colleagues. http://another-ro.com/forum/viewtopic.php?id=150435
Do you mind if I quote a few of your articles aas
long as I provide credit annd sources back to your website?
My blog is in the exact same area of interest as yours and my visitors would realy benefit frlm some of the information yyou present here.
Please let me know if this alright with you. Thanks! https://camillacastro.us/forums/viewtopic.php?id=327778
Whhen I originally commented I clicked the
“Notify me when new comments are added” checkbox and now each
tiime a comment is added I get four emails with the same comment.
Is there any way you caan remove people from that service?
Thanks! http://forum.altaycoins.com/viewtopic.php?id=695950
Great post. I was checking continuously this blog and I am impressed!
Extremely helpful information specially the lsst part :
) I care for such info much. I was looking for ths particular info
for a long time. Thank you and best of luck. http://another-ro.com/forum/viewtopic.php?id=152063
constantly i used to read smaller contemt which ass well clear their motive, and that is also happening with this podt which I am reading
at this time. https://camillacastro.us/forums/viewtopic.php?id=327927
Hello there! I know this is kinda ooff topic nevertheless
I’d figured I’d ask. Would you be interested in exchanging links or maybe
guest writing a blog post or vice-versa? My site goes over a lot of thhe same
topics as yours and I think we could greatly benefit fropm each other.
If you’re interested feel free to send me an e-mail. I look forward to hearing from you!
Great blog by the way! http://another-ro.com/forum/viewtopic.php?id=152058
Thanks for finally talking about >Paain management –
through the psychological lens | PsychWorks Associates <Loved it! http://forum.ainsinet.fr/profile.php?id=351743
You are so cool! I do not think I have read anything likke that before.
So nice tto discover somebody with a few genuine thoughts on this subject matter.
Seriously.. many thanks for starting this
up. This web site is something thaat is required on the internet,
someone with a little originality! https://www.alonegocio.net.br/author/patrice5868/
Excellent waay of explaining, and nice article to get information concerning my presentation subject, whicxh i amm going to pressnt in academy. http://forum.altaycoins.com/viewtopic.php?id=695212
Hello, after reading this awesome post i am also
cheerful to share my knowledge here with friends. http://forum.altaycoins.com/profile.php?id=473772
Do you have a spam issue on this website; I also am
a blogger, and I was wanting to know your situation; we have created
some nice ppractices and we are looking to swap solutions
wiith others, please shoot me aan email if interested. http://forum.altaycoins.com/viewtopic.php?id=693792
Great web site you’ve got here.. It’s difficult to find quality writing like yours nowadays.
I seriojsly appreciate ppeople like you! Take care!! https://advansbum.by/component/k2/itemlist/user/888317
I visited multiple blogs but the audio quality for
audio songs current at this site is eally superb. https://camillacastro.us/forums/profile.php?id=170018
Thanks for sharing your thoughts about casino. Regards https://bicycledude.com/forum/profile.php?id=1523043
You arre so awesome! I do not believe I’ve truly read through anything like
hat before. So great to fimd somebody with a few genuine thoughts on this topic.
Seriously.. many thanks for starting this up.
Thiss site is one thing that’s needed on the web,
someone with a little originality! https://www.mazafakas.com/user/profile/4176039
Hi! I’ve been following your site for a long time noww and finally
got the courage to go ahjead and give you a shout out frtom Huffman Tx!
Jusst wanted to say keep up the good job! https://www.alonegocio.net.br/author/danielegfz5/
I’m truly enjoying tthe design and layout of your website.
It’s a very easy on the eyes which makes it much more enjoyable
for me to come here andd visit more often. Didd you hire out a developer to create your theme?
Great work! http://links.musicnotch.com/colleentqd20
Howdy I am sso glad I found your site, I really found yoou byy error, while I was browsing on Google for something else, Anyhow I am here now and wwould just like to say kudos for
a fantastic post and a all round entertaining blog (I alo love thhe theme/design), I don’t have time too read it all at the
moment but I have saved it and also added in your RSS feeds,
so wuen I hhave time I will be back to read a lot more, Please do kep upp the great work. http://alpervitrin40.xyz/author/rosalievarl/
Hi, I think your site might be having browser compatibility issues.
When I look at your website in Chrome, it looks fine but when opening in Internet Explorer, it has some
overlapping. I juyst wanted to give you a quick heads up!
Other then that, awesome blog! http://forum.ainsinet.fr/profile.php?id=351986
I am actually delighted to glance at this web site posts which
includes lots of useful data, thanks forr providing these data. http://forum.altaycoins.com/profile.php?id=474115
This informkation is priceless. Whhen can I find out more? http://forum.altaycoins.com/viewtopic.php?id=693512
Hmm is anyone else encountering problems with the ictures on this blog loading?
I’m trying to determine if its a problem on my end
oor if it’s the blog. Any suggestions would be greatly appreciated. https://camillacastro.us/forums/viewtopic.php?id=327466
Great info. Lucky me I discoveredd your website by accident (stumbleupon).
I’ve saved as a favorite for later! https://bicycledude.com/forum/profile.php?id=1524128
Good day! Do you knnow if they make any plugins to safeguiard against hackers?
I’m kinda paranoid about losing everything I’ve worked hard on. Any suggestions? http://forum.altaycoins.com/profile.php?id=474104
I loved as much as you’ll receive casrried out right here.
The sketch is tasteful, your authored matefial stylish.
nonetheless, you command get got an edginess over that you
wish be delivering the following. unwell unquestionably come more formerly atain as exactly tthe same nearly
very often inside case you shield this hike. http://another-ro.com/forum/viewtopic.php?id=152125
Helpful information. Lucky me I discovered your site accidentally, and I’m surprised why this twist of fate didn’t took place
earlier! I bookmrked it. https://www.mazafakas.com/user/profile/4175755
Its like you read my mind! You seem to know so much about this, like you wrote the book in it or something.
I think that you can do wigh a few pics to drive the message home a bit, but instead of that,
this is magnificent blog. A great read. I will definitely be back. https://advansbum.by/?option=com_k2&view=itemlist&task=user&id=888408
Thanks to my faather who shared with me concerning this
webpage, this wwebsite is genuinely amazing. http://links.musicnotch.com/corinnecheng
I used to be recommended this blog via my cousin. I am no longer positive whether
this publish is written by him as no one else recognize such unique
approximately my trouble. You are incredible! Thanks! http://www.ozsever.com.tr/component/k2/itemlist/user/406215
Quality poksts is the important to interest the
visitors to pay a vvisit the web site, that’s what this web page is providing. http://another-ro.com/forum/viewtopic.php?id=150726
Wonderful article! We are linking to this particularly great post
on our site. Keep up the great writing. http://forum.altaycoins.com/viewtopic.php?id=696129
I do not eveen know how I endeed up here, but I
thought this post was great. I do not know who you are but definitely yyou are going
to a famous blogger if you are not already 😉 Cheers! http://another-ro.com/forum/viewtopic.php?id=150613
I’m not that much of a online reader to be honest but your blogs really nice, keep it up!
I’ll go ahead andd bookmark your site to come back later.
Many thanks https://telegra.ph/What-is-the-Difference-between-a-Nonprofit-Organization-and-a-Charity-05-22-2
No matter if some one searches forr his required thing,
therefore he/she needs to bbe available that
in detail, so that thing is maintained over here. https://charitables9.wordpress.com/
Undeniably imagine that that youu stated. Yoour favorite justification seemed to bee on thhe weeb the simplest thing to have in mind of.
I say to you,I certainly get irfked whilst other peolle consider issues that they plainly don’t know about.
You controlled to hit the nail upon the top as neatly as outlined out the whole thing wthout
having side effect , other peoplpe could take a signal. Will probably be back
to gget more. Thank you https://telegra.ph/Difference-between-a-Nonprofit-Organization-and-a-Charity-05-22
I do not create a leave a response, however after reading through a few of the
responses here Pain management – through the psychological lens | PsychWorks Associates.
I actually do have a couple of questions for you if you do noot mind.
Is it just mme or does it give thee impression like some of
thhe comments look like they are eft by brain dead people?
😛 And, if you are posting at additional sites, I’d like
to follow anything fresh youu have to post.
Could you list of every onee of your social sites like your
twitter feed, Facebook page or linkedin profile? https://telegra.ph/What-is-the-Difference-between-a-Nonprofit-Organization-and-a-Charity-05-22
I really love your blog.. Gret colors & theme.
Did you create this web site yourself? Please reply back ass
I’m trying to create my own personal site
and want too knmow where you got this from or exactly what the theme is called.
Manyy thanks! https://communitysupport.mystrikingly.com/
Great blog here! Additionally your web site so much up
very fast! What web host are you using? Can I am getting your associzte hyperlink on your host?
I want my website loaded up as quickly as yours lol https://telegra.ph/Top-5-developments-driving-growth-for-video-games-05-22
I am really enjoying the theme/design of your weblog. Do
yyou ever run into any web browser compatibility issues?
A number of my bloog audience have complained about my blog nott working correctly in Explorer buut looks great in Chrome.
Do you have any solutions to help fix this issue? https://664e0c7b18aee.site123.me/
I am not sure where you’re getting your information, but good topic.
I needs to spend some time learning more or understanding more.
Thanks for agnificent info I was looking for this info for myy mission. https://664e0e8f1b541.site123.me/
Amazing! Its in fact amazing article, I have got much clear idea about
from this article. https://gametrendss.mystrikingly.com/
Fantastic items from you, man. I’ve understand your stuff
previous to and you are just extremely great. I actually like
what you have boutht right here, really like what you’re saying and the way during which you are saying
it. You make it enjoyable and you continue to take care off to stay it wise.
I can’t wit to read far moree from you. This is really a tremendous website. https://worldsports.mystrikingly.com/
What’s Happening i am new to this, I stumbled upon this I have found
It absolutely seful and it has aided me out loads.I hope to give a contribution & aid other
users like its helped me. Great job. https://topsportevents.blogspot.com/2024/05/top-10-most-watched-sporting-events-in.html
Yes! Finally someone writes about casino. https://sporttopevents.blogspot.com/2024/05/top-10-most-watched-sporting-events-in.html
These arre truly great ideas in concerning blogging. You have
touched some fastidious things here. Anny way keep up wrinting. https://telegra.ph/Viewable-History—Five-Most-Watched-Sporting-Events-In-the-World-05-23
It’s fantastic that you are gettijng ideas from this pst as well as from our discussion made here. https://664e14fb3ed61.site123.me/
What’s up, after reading this remarkable post i am as well happy tto share
my familiarity here with friends. https://topsports.mystrikingly.com/
Wow! In the end I got a web site from where I be capable of really take valuable facts concerning my study and knowledge. https://moderntechs.mystrikingly.com/
Excellent blog here! Also your site loads up very fast!
What host are you using? Can I get your affiliate link tto your host?
I wish my site loaded up as quickly as yours lol https://newtop5technology.blogspot.com/2024/05/breakthroughs-that-change-our-lives.html
Its such as you learn my thoughts! You appear to grasp so much approximateky this, such as yyou wrote the
book in it or something. I believe that you just could do with
a few pedcent to drive the message home a bit, however other than that,
this is great blog. A fantastic read. I’ll certainly bbe back. https://newtech02.wordpress.com/
Hi, I read your blog daily. Yoour story-telling style is awesome, kedp
up the good work! https://664f4ab5a3927.site123.me/
Oh my goodness! Impressive article dude! Thanks, However I am experiencing probhlems
with your RSS. I don’t understand why I cannot subscribe to it.
Is there anyone else getting the same RSS issues? Anybody who
knows the answer can you kindly respond? Thanks!! https://topnewtechs.mystrikingly.com/
Hey this is somewhat oof off topic but I was wanting to know
if blogs use WYSIWYG editors or if you have to manually code with HTML.
I’m starting a blog soon but have no coding know-how so I wanted tto get
advuce from someone with experience. Any heop
would be enormously appreciated! https://toptechs.mystrikingly.com/
Normally I don’t learn artice on blogs, but I would like to
say that this write-up very forced me to try and do it!
Yoour writing style has been amazed me. Thanks,
very great post. https://traveltoptips6.wordpress.com/
These are truly fantastic ideas in concerning blogging.
You have touched some pleasant factoors here.
Any way keep up wrinting. https://gowildtravel.blogspot.com/2024/05/how-to-do-serious-nature-and-wildlife.html
Yoou really make iit seem so easy with your presentation butt I find this topic to
be actually somethingg which I think I wokuld nevr understand.
It seems too complicated and extremely bropad for me.
I’m looking forward for your next post, I will try to get the hang of it! https://wildtravels9.wordpress.com/
Fantastic items from you, man. I have have in mind
your stuff previous to and you’re sijmply extemely excellent.
I actually likee what you have bought right here, certainly like wat you’re stating and the
way in which during which you assert it. You are making it enjoyable and you still take care
of to sfay it smart. I cant waiit to learn far more from you.
Thhis is actually a tremendous site. https://telegra.ph/Guide-to-Wildlife-Travel–Everything-You-Need-to-Know-05-23
Pretty component of content. I just stumbld upon your site and in accession capital to say that
I get in fact enjoyed account your wesblog posts. Any waay I
wkll bbe subscribing foor your augment or even I achievement you get admissionn to constantly
quickly. https://future-techss.blogspot.com/2024/05/10-inspiring-graphic-design-trends-for.html
Hi there i am kavin, its my first time to commenting anyplace, when i read this article i
thought i could also create comment due to this brilliant piece
oof writing. https://telegra.ph/Top-11-Graphic-Design-Trends-for-2024-The-Future-of-Visual-Communication-05-23
Thank you for every other magnificent post. Where else may
anybody get that type of information in such a perfect method of writing?
I’ve a presentation next week, and I am aat the search for such information. https://graphicdesign2024.wordpress.com/
Your stule is unique compared to other follks I have rread stuff from.
I appreciate youu for posting when you’ve got tthe opportunity, Guess I’ll
just bookmark this site. https://664f66eced7c3.site123.me/
bactrim 1
doxycycline 75 mg
Just wish to say your article is as astounding.
The clearnhess in your post is simply great and i could
assume you’re aan expert on this subject. Fine with your permission let me
to grab your feed to kewp up too date with forthcoming post.
Thanks a million and please keep up the gratifying work. https://www.deviantart.com/ruth5555/journal/The-impact-of-technology-on-the-future-of-gambling-1024700212
Yes! Finally someone writes about casino. https://www.uworld.com/forum/messages.aspx?TopicID=51616&gid=1
Thanks ffor another great article. The place else may anyone gget that kind of
information in such a perfect method of writing?
I’ve a presentation subsequent week, and I’m at the search for such information. https://www.themoviedb.org/u/AviatorGames
Youu ctually make it appear so easy with your presentation however I iin finding this
matter to be really one thing which I think I’d never understand.
It sort of feels too complex and very large for me. I’m having a look ahjead for your next put up, I’ll attempt tto get the hang oof it! https://medium.com/@gustaveguertin979/the-impact-of-gambling-regulation-on-the-online-casino-market-b710da4a3876
Wow! After all I got a weblog from where I can actually get vwluable
information concerning my study aand knowledge. https://pixabay.com/users/aviatorgame-43890672/
It is appropriate time to make a few plans for the long run annd it
is time to bbe happy. I’ve read this publish andd if I could I wwish to recommend you some attention-grabbing hings or suggestions.
Perhaps you can write subsequent articles regarding this article.
I desire to learn more issues about it! https://www.walkscore.com/people/127538447471/gavin-ward
awesome
baclofen 25mg tablets
buy lyrica online from mexico
acyclovir 200
where can you get accutane online
Hi, I do believe yoour website could be having web browser compatibilty issues.
Whenever I take a look at your blog inn Safari, it looks fine however when opening in I.E., it has some overlapping issues.
I merely wanted to provide you with a quick heads up!
Aside fom that, wonderful site! https://www.dantellahome.com/2024/06/20/the-secret-of-essay-writing-that-no-one-is-talking-about/
Good post. I learn something totally new and challenging on sitges I stumbleupon every day.
It’s always helpful to read content from other writers and practice a little smething ffrom their websites. https://findbestserver.com/9-diy-essay-writing-ideas-you-will-have-missed/
Greate post. Keep posting such kin of info on your page.
Im realy impressed bby it.
Hey there, You have performed an excellent job. I will certainly digg it and for my pardt suggest too my friends.
I am sure they will be benefited fro this website. http://www.annunciogratis.net/author/qmpkathy983
Howdy! I know this is kinda offf topic but I wass wondering which bog platform aree you using for this site?
I’m getting sick and tired of WordPress because I’ve had
issues with hackers and I’m looking at alternatives
for another platform. I would be great iff you could point me in the direction of a good platform. https://www.pitstopodium.com/f1-news/facts-fiction-and-essay-writing/
Hey very interesting blog! https://casajienilor.ro/seven-things-to-demystify-essay-writing/
WOW just what I was looking for. Came here by searching for essay https://findbestserver.com/type-of-essay-writing/
Prtty nice post. I just stumbled upon your weblog and wanted
to say that I have really enjoyed browsing your bllg posts.
After all I’ll be subscribig to your rss feed and I hope you write
again very soon! https://affiliates.trustgdpa.com/essay-writing-cash-experiment/
Hi there! I just want to offer you a big thumbs up for
your excellent info you have hhere on this post.
I am returning to ylur website for more soon. https://casajienilor.ro/death-essay-writing-and-taxes-tips-to-avoiding-essay-writing/
Hi there, I enjoy reading through your article. I wanted to write a little comment to support you. https://ladder2leader.com/open-mike-on-essay-writing/
buy cheap sildalis
order retin a without prescription
flomax medication coupon
cialis 10mg price canada
baclofen gel
baclofen 2 cream
lioresal
furosemide medicine 20 mg
cialis for daily use cost
https://www.instagram.com/asiapsiholog_family/
where can i buy lasix online
tamoxifen sale online
modafinil 100mg
lasix generic cost
Vivez les programmes suisses comme jamais auparavant possible avec notre service IPTV de qualité supérieure !
Accédez librement aux chaînes suisses favorites comme la RTS, SRF, RSI et bien d’autres. Notre service offre :
Plus de nombreuses chaînes suisses et étrangères en résolution haute
Un choix VOD riche en films et émissions
La option de regarder vos émissions préférées en différé
Une interface intuitive qui marche avec divers dispositifs
Un assistance client rapide situé en Suisse
Que vous soyez passionné de sport, de nouvelles ou de programmes de variété, notre service IPTV
Abonnement IPTV – La nouvelle révolution du divertissement à domicile s’adapte à vos besoins. Profitez d’un essai gratuit pendant 24 heures et découvrez une façon innovante de voir la télévision !
how to buy accutane online
I am a casino online that has shared my information on how to make money online, This is not a scam but my knowledge of how to play.
https://main7.top
https://epicads.net/
шкаф для раздевалок практик стандарт ls 21 60 https://office-mebel-in-msk.ru/
tretinoin tablets price
купить справку
Vivez la télévision suisse comme jamais expérimentée avec notre offre IPTV de première qualité !
Bénéficiez d’un accès sans limites aux chaînes suisses favorites comme RTS (Radio Télévision Suisse), SRF (Schweizer Radio und Fernsehen), RSI (Radiotelevisione svizzera) et bien d’autres. Notre plateforme offre :
Plus de 100 chaînes locales et internationales en qualité HD
Un sélection VOD riche en films et séries
La faculté de revoir vos émissions préférées
Une interface conviviale qui marche avec divers dispositifs
Un support client dynamique situé en Suisse
Que vous soyez enthousiaste de sport, d’informations ou de spectacles, notre service IPTV
Blog Freely – IPTV Smarters Pro, votre application TV préférée
s’adapte à vos préférences. Profitez d’un essai gratuit pendant une journée et découvrez une nouvelle manière de visionner la télé !
Обязательно попробуйте обратиться к gazon-msk, их специализация это газоны в рулонах, они знают свое ремесло
Hi! This is kijd of off topic but I need some advice from an established blog.
Is it tough to set up yopur own blog? I’m not very techincal but I can figure hings out prettty fast.
I’m thinking about creatring my own but I’m not sure where to start.
Do you have anyy tips or suggestions? Thank you https://www.chordie.com/forum/profile.php?id=1988133
If you are goiong for most excellent ontents like I do, just
goo to see this web site everyday for the reason that it offers feature contents, thanks https://linktr.ee/aviatorsgames
If sopme one needs to be updated with most up-to-date technologies then he must be visit tis site and bbe up to dqte everyday. https://www.provenexpert.com/en-us/aviator-game3/
I’ve been surfing online more than 3 hours today, yet I never found any innteresting article likke yours.
It iss pretty worth enough for me. In my view, if all sit owners aand bloggers
msde good content as you did, the net will be a lot morte useful than eve before. https://telegra.ph/Exploring-the-Thrills-of-Gambling-on-Special-Events-Poker-Roulette-Blackjack-and-Beyond-11-11
It is the best time to make some plans for the long run and it’s time to be happy.
I have learn this put upp and if I could I wish to suggest you few interesting issues
or tips. Maaybe you can write subsequent articles referring to this article.
I wish to read even more things approximately it! https://www.provenexpert.com/en-us/aviatorgamedemo/
Howdy would you mind stating whic blog platform you’re
working with? I’m going to staret myy own blog in the near future but I’m
having a difficult time selecting between BlogEngine/Wordpress/B2evolution and Drupal.
The rdason I ask iss because your layout seems
different then most blogs and I’m looking for something unique.
P.S My apologiies for being off-topic bbut I had to ask! https://vocal.media/authors/haments87
Amazing! This blog looks exactly like mmy old one! It’s on a completely different
topic but it has pretty much the same layout and design. Wonderful choice of colors! https://www.horseracingnation.com/user/aviatorgame
This paragraph offers clear idea iin support of the new users off blogging, tthat actually hhow to do blogging and
site-building. https://www.walkscore.com/people/313322142039/walter-diaz
Very rapidly this wweb page will bee famous amid all
blogging and site-building viewers, due to it’s fastidious articles or reviews https://www.themoviedb.org/u/Aviator1
https://new.gruz200.kz/
generic lyrica online
центр ремонта телефонов
починить смартфон
вавада казино зеркало
Hey I know this is off topic but I was wondering if you knew of any widgets I could add
to myy blog that automaatically tweet mmy newest twitter updates.
I’ve been looking for a plug-in like this for quite some time
and was hoping maybe you would have some experience with something like this.
Please let me know iif you run into anything. I truly enjoy reaing your blog and I look forward to your neww updates. https://forum.pgbu.ir/viewtopic.php?id=563
Wow, that’s what I was seeking for, what a material!
present here at this website, thanks admin of this web page. https://careked.com/community/profile/aimeemzo4098967/
I’ll immediately clutch your rss as I can not find your email subscription hyperlink or e-newsletter service.
Do you have any? Kindly allow me realize so that I could subscribe.
Thanks. https://stemacumen.net/blog/index.php?entryid=2748
I drop a comment whenever I like a post on a site
oor if I have something to contribute to
the conversation. Usually it is caused byy the sincerness communicated in the article I looked at.
And after this post Pain management – throufh the psychological lens | PsychWorks
Associates. I was actually moved enough to leave a thought
🙂 I actually do have 2 questions for you if it’s okay. Is it only me or does it
look as if like a few of the responses appear as if they are written by brain dead folks?
😛 And, if you are posting at additional online social sites,
I’d like to follow you. Could you maake a listt all of all your community pages like your linkedin profile, Facebook
page or twitter feed? https://robertsspaceindustries.com/citizens/lauracasey
Quality articles or reviews is the secret to interest the people to visit the site, that’s what
this wweb page is providing. https://stemacumen.net/blog/index.php?entryid=2758
Pretty component to content. I simply stumbled upon your site and
in accession capital to assert hat I get actually enjoyed acount your weblog
posts. Anyway I’ll be subscribing to your feeds and even I achievement
you access persistently rapidly. https://www.camedu.org/blog/index.php?entryid=57642
An impressive share! I have just forarded this onto a friend who has been doig a little homewprk oon this.
Andd he actually ordered me lunch due to the fact that I discovered it for
him… lol. So allow me to reword this…. Thank YOU forr the meal!!
But yeah, thznx for spending soke time to talk about this subject here on your blog. https://forum.pgbu.ir/viewtopic.php?id=617
Pretty nice post. I just stumbled upon your blo and wanted to ssay
that I’ve truly enjoyed surfing around your blog posts. After all I’ll be subscribing to our
rss feed and I hope you writee again very soon! http://demo.qkseo.in/viewtopic.php?id=834561
Excellent goods from you, man. I’ve ujderstand your stuff previous tto and you are just tooo wonderful.
I really like what you have acquired here, cerrtainly like what you are stating andd the wayy
in which you ssay it. You make it enjoyable and you
still care ffor to keep it smart. I cant wait to read much more from you.
This is really a great web site. https://knowledgekh.com/blog/index.php?entryid=5666
ремонт смартфонов в москве
скачать zenit
навес двухскатный
buy viagra medicine online india
сервис ремонта мобильных телефонов
мастерская по ремонту ноутбуков
ремонт мониторов
augmentin over the counter
раковина над стиральной
купить справку
clomid tablet online india
ремонт мобильных телефонов в москве
https://vskrytiyezamkov.ru/
сервис ремонта мобильных телефонов
toradol for kidney stones
про офис мебель https://office-mebel-on-msk.ru/
Bitcoin tumbler
http://intermedservice.ru/vazhnost-zabotyi-o-svoem-zdorove/
купить газоблоки для строительства https://gazobeton-moskow.ru/
locowin casino
אביב, לפעמים קשה למצוא את המילים שמתארות את החוויה. נעים, מענג, מעורר, משחרר, מדהים ובלתי נשכח הם חלק מהמילים שבהם גברים לבוא. ולקבל אותם מתי שרוצים. ואנחנו יודעים שזה מה שאתה רוצה ברגע זה. ואין שום בעיה, הנערות תמיד זמינות לתת שירות. ניתן למצוא נערת ליווי באר שבע
לראווה גוף מושלם, והן גם משתמשות בגוף הזה בשביל לפנק ולענג אותך ללא גבולות. אתה יכול להזמין נערות ליווי בחיפה 24 שעות ביממה, לחוץ מכל מה שקורה מסביב – יש לנו את התשובה בשבילך. כל מה שאתה צריך לעשות זה פשוט להזמין נערות ליווי בתל אביב ולהתחיל לבלות. הן סקס נשים
וחרמנים שעדיין גרים עם ההורים, ואין להם פרטיות. דירות דיסקרטיות בבאר שבע פותרות לכולם את הבעיות. זהו גם הבילוי שכל גבר משתוקק דיסקרטיות בתל אביב ונהנים מהחוויה המתוקה והמשחררת. ניתן למצוא דירות ממש מעבר לפינה, והן מציעות לגברים סביבת בילוי בטוחה עם look at this website
baclofen 159
ולבלות איתם. והן מחכות שאתה תתקשר ותקבע. דירות דיסקרטיות בחיפה הן מקום שבו אתה יכול למצוא את השקט שלך 24 שעות ביממה ו 7 ימים גדול ועור רך ונעים כפי שאתה אוהב. ואלו הם הכלים באמצעותם נערות הליווי מפנקות את הגברים וגורמות לגבר להרגיש טוב. בילוי דיסקרטי great link
להרגיש כמו כוכב פורנו, ולבלות עם בחורות בעלות גוף מחרמן, בוא לבלות. יש דירות דיסקרטיות בתל אביב, והן זמינות 24 שעות ביממה. להציע, כדאי לך לבוא לבקר עוד היום בדירות הדיסקרטיות. דירות דיסקרטיות בבאר שבע הן המקום למצוא את מה שאתה מחפש. כאשר תגיע לבקר related site
Glory Casino
buy metformin online australia
לבילוי מפנק ואינטימי סצנת הבילוי של חיפה היא לא רק מועדונים וברים טרנדיים, היא כוללת גם נערות ליווי בחיפה. זהו שירות או אולי גברים המחפשים קצת אטרקציות למסיבת הרווקים. לכל אחד יש את הסיבות שלו, אבל האמת שזה לא ממש משנה. נערות ליווי בחיפה לא check out your url
ללמוד דברים חדשים, או אולי להפתיע אותן בדברים חדשים ונועזים, זוהי ההזדמנות שלך. לא בכל יום פוגשים בחורות כל כך יפות שפשוט יודעות כיצד לגרום לך לשכוח מכל הצרות ומכל הבעיות, והן זמינות בכל יום ובכל שעה. הצטרף גם אתה לרשימת הגברים הנהנים מהשירות דירות דיסקרטיות אתיופיות
שכל אחת מציגה גוף מהסרטים, היא גם יודעת להפוך אותך לכוכב של הסרט. אתה תוכל לעשות מה שאתה רוצה והנערה תזרום איתך. ולא משנה מה דיסקרטיות בתל אביב ונהנים מהחוויה המתוקה והמשחררת. ניתן למצוא דירות ממש מעבר לפינה, והן מציעות לגברים סביבת בילוי בטוחה עם look here
מזמינים את הנערות היפות, הן נותנות את כל מה שהן יכולות על מנת לגרום לגבר עונג. הן משתמשות בכל גופן על מנת לרגש את הגבר. ויש להן רוצות שהגבר ירגיש כמו מלך. אתה יכול להזמין נערות ליווי בתל אביב ולגלות יחדיו את העולם הנפלא של הגשמת הפנטזיות. לגלות יחדיו את browse around these guys
זהו שירות המספק את הצרכים של הגוף הגברי ואת המהות של להיות גבר. בילוי עם נערות ליווי בתל אביב מאפשר לגבר להשתחרר ולהתפרק. זוהי המארחות גברים בדירתן. דירות דיסקרטיות בתל אביב הן הפתרון לכל מי שבמקרה עבר בסביבה והתחשק לו לבלות. אולי זה גבר שהגיע לכל מיני חדרים לפי שעה
המחפשים דיסקרטיות – כולם מגיעים אל דירות דיסקרטיות בתל אביב. המקום בו ניתן למצוא רוגע, פורקן ורגעים מלאים באהבה ותשוקה. זהו אתה תוכל ליהנות מגופן במהלך בילוי אינטימי עמוק ובלתי נשכח. זהו בדיוק הבילוי שאתה צריך עכשיו, זה מה שהגוף שלך מבקש עכשיו. נערות my company
Кавказская мазь https://kavkazmaz.ru для суставов купить в аптеке. Официальный сайт производителя Кавказской мази от боли в суставах.
מלאים. נערות ליווי בתל אביב הן ההזדמנות שחיפשת בשביל להגשים את עצמך ואת כל החשקים שלך. זוהי ההזדמנות לעשות את כל מה שחלמת עליו אם בא לך לראות במה מדובר, ולהרגיש חלק מאותו מועדון אקסקלוסיבי של גברים, הזמן את הנערות הסקסיות ותגלה במה מדובר. זהו בילוי שכל navigate here
האקסקלוסיבי. אנשי עסקים מהארץ ומחוץ לארץ, וגברים רווקים ונשואים, אלמנים וגרושים, מבלים עם הנערות ונהנים מהשירות ברמה הגבוהה. כאשר יש בילוי או מסיבה, ורוצים להרים את מצב הרוח אפשר תמיד להזמין אותן. גברים אוהבים להגשים את החלומות שלהם. וזה נכון גם כאשר נערות ליווי בחיפה
Чудо Гриб препарат от паразитов https://chydogrib.ru и ВПЧ. Купите средство по минимальной цене, изучите отзывы и инструкцию по применению.
https://derbayerischelowe.info/
baclofen mexico